December 8, 2007
Please, know your rights!
These laws provide all patients, pregnant or not, with certain fundamental rights:
The right to exercise self-determination and autonomy in making all medical decisions, including the decision to refuse treatment.
The right to bodily integrity. Any form of non-consensual touching or treatment that occurs in a medical setting constitutes battery.
The right to be provided with the necessary information on which to base medical decisions, including a diagnosis; recommended treatments and alternatives; the risks, benefits, discomforts and potential disabilities of proposed medical treatments; realistic expectation of outcomes; a second opinion; and any financial or research interests a physician may have in proposing certain treatments.
The right to be informed of any potentially life-threatening consequences of a proposed treatment, even if the likelihood of experiencing such and an outcome is rare.
The right to make medical decisions free from coercion or undue influence from physicians.
The right to have informed medical decisions witnessed, signed, and documented by the attending physician and another adult.
The right to revoke consent to treatment at any time, either verbally or in writing.
Source: Born in the USA by Marsden Wagner
December 7, 2007
The "Business" of Birthing in the US
Note: All of the information here represents fact, not opinion, of birthing within the United States. If you don't believe it, check the references listed at the end of the article. That being said, you may want to sit down before reading further...
FACT
Each year, the U.S. spends over $50 billion dollars on childbirth. This is more than any other nation in the world. (This number does not include babies in the NICU or readmissions during the first month.)
FACT
Birthing is the largest source of income for American hospitals.
FACT
The U.S. ranks 37th in the world for the quality of its health care.
FACT
Over HALF of all hospital admissions in America are for maternity.
FACT
Hospitals are NOT the safest place to have a baby. 25 infectious strains exist that are resistant to ALL known antibiotics. These are found primarily in hospitals.
FACT
75 years of routine hospital birth have produced NO studies to show it is safer than having a baby at home.
FACT
Both homebirth and birth centers have been scientifically proven to be safer than hospitals with a skilled labor attendant (i.e. midwives, not doctors).
FACT
The more technology used in childbirth, the more dangerous it becomes.
FACT
The larger the hospital, the greater the risks to both mother and baby.
FACT
Of the 4.3 million babies born annually in the U.S., a mere 5% represent natural childbirth.
FACT
America has the 32nd highest infant mortality rate in the entire world.
FACT
The U.S.A. has the 14th highest maternal mortality ratio among developed nations.
FACT
Over 90% of all infants in the U.S. are born with drugs (e.g. narcotics from epidurals, pitocin, acetaminophen, etc) in their systems. NONE of these drugs have been tested for safe use in infants.
FACT
A 24-hour hospital stay, uncomplicated delivery in the U.S.A. costs anywhere from $8,000-10,000. This cost DOUBLES for a c-section.
FACT
ALL families in the U.S. are charged newborn nursery charges, even if the baby NEVER leaves the mother's room. This "routine" charge amounts to about $1.3 billion dollars annually, for services that are NOT rendered. (I'm not quite sure why this doesn't constitute insurance fraud - billing for services not rendered.)
FACT
Every year, 1 million, or about 20%, full-term, healthy infants are sent to the NICU for "observation" for an average stay of 3 days, totaling a whopping $6,000.
FACT
For newborns suspected to have serious medical conditions, the same NICU stay totals $20,000.
FACT
1 in 3 American women has an episiotomy. Episiotomies are medically indicated for less than 10% of all women. Over 1 million unnecessary episiotomies are performed annually in the U.S.
FACT
1 in 5 births in the U.S.A. are induced. 44% of women surveyed in 2002 reported their doctor wanted to induce. Only 16% reported medically-indicated reasons.
FACT
American women who elect epidurals are FOUR times as likely to have cesarean sections.
FACT
1 in 4 American babies are born by cesarean section. The World Health Organization recommends a c-section rate of less than 10% as acceptable.
FACT
U.S. hospital policies for routine tests, practices, policies and procedures are based on financial considerations, which include malpractice insurance costs. They are not based on evidence, research, or appropriateness of care.
I truly hope you found these statistics disturbing. If they don't speak to the medicalization of childbirth in this country, I don't know what does.
The true horror comes in the fact that these views are being exported across the world. As the U.S. is such a powerhouse of marketing, more impressionable regions are adapting to these customs, despite the overwhelming evidence that the U.S. approach to childbirth IS SERIOUSLY FLAWED!
American obstetricians are taught to view birth as "a disaster waiting to happen." The average delivery in the U.S. is neither natural nor healthy. We have embraced a cascading system of successively more intense, unneeded interventions termed "active management" or the "standard of care".
So what do we do? How can we change the system?
We as a country need to reach beyond our own boundaries to embrace an effective model of maternity care. We, as women, mothers, and families, must educate ourselves as to the true process of labor and birthing.
We must regain our faith in our bodies' perfect ability to have a baby. We must look at what the research is already telling us - that nature has it right!
In short, we must take back our birthing!
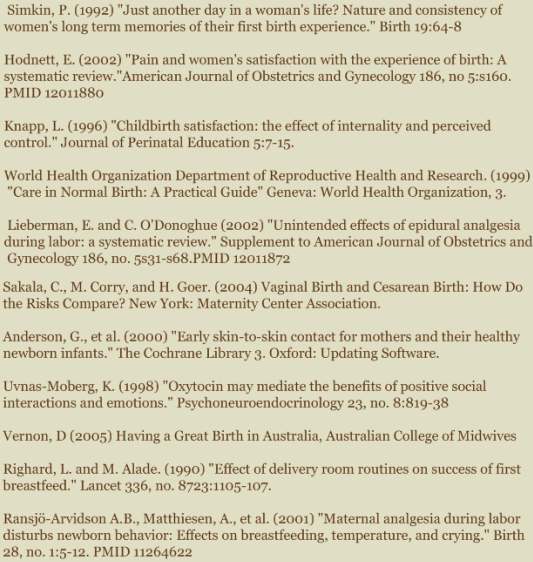
And if you're still not convinced, check these out:
From Giving Birth Naturally dot com http://www.givingbirthnaturally.com/birthing.html
2007 Cesarean Research Results
The cesarean rate as of 2006 was 31.1% as a nation...sick. The WHO (World Health Organization) recommends rates no higher than 15%...what gives USA?
Rising Cesarean Rate Bad for Mothers
Top 12 Studies from 2007
Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study (Villar, et al., British Medical Journal, 2007;335:1025, 17 November)
Study Design: Researchers assessed the risks and benefits of cesarean delivery vs. vaginal delivery.
Bottom line: Cesarean carries twice the risk of injury and death for both mother and baby. Women with cesarean experience double the rate of hysterectomy, blood transfusion, admission to intensive care, prolonged hospital stay and death, compared to mother who delivered vaginally. Babies born by cesarean were 45 percent more likely to be in the neonatal intensive care unit for 7 days and 41-82 percent more likely to die than babies born vaginally.
Risk of Uterine Rupture and Adverse Perinatal Outcome at Term After Cesarean Delivery (Spong, et al., Obstetrics and Gynecology 2007; 110: 801-7)
Study Design: Researchers examined the risk of uterine rupture after cesarean and what harms it may have for mothers and babies.
Bottom line: Regardless of how the baby was delivered, the rate of uterine rupture was low and complications from rupture were also low for both mother and baby.
Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. (Declercq, et al. American Journal of Obstetrics and Gynecology. 2007 Mar; 109(3):669-77.)
Study Design: Researcher divided mothers into two groups: women with a planned cesarean after no labor and women who labored and had either a cesarean or vaginal birth and then compared rehospitalization rates.
Bottom Line: Rehospitalizations in the first 30 days after giving birth were 2.3 times more likely in planned cesarean than with planned vaginal births. The leading causes of rehospitalization after a planned cesarean were wound complications and infection. Hospital costs were 76 percent higher for women with planned cesarean, and hospital stays were 77 percent longer.
Previous caesarean or vaginal delivery: Which mode is a greater risk of perinatal death at the second delivery? (Richter, et al., European Journal of Obstetrics & Gynecology and Reproductive Biology 2007; 132: 51-7)
Study Design: Researchers compared mothers who had delivered previously by cesarean vs. vaginally, and examined the number of babies who died in the subsequent pregnancy.
Bottom line: A previous cesarean delivery was associated with a 40 percent increase in perinatal death (the first week after birth) and a 52 percent increase risk of stillbirth. A vaginal or cesarean delivery in the current pregnancy did not impact the death rate.
Postcesarean delivery adhesions associated with delayed delivery of infant (Morales, et al., American Journal of Obstetrics and Gynecology 2007; 196: 461.e1-e6
Study Design: A common complication of any surgery is overgrowth of scar tissue, called “adhesions.” Researchers examined the frequency of adhesions with successive cesareans and whether adhesions caused by cesareans could slow down the delivery of a baby in the next pregnancy.
Bottom line: Researchers concluded that each successive cesarean significantly increases the incidence of adhesions and can slow down the delivery of a baby. One prior cesarean adds 5.6 minutes to the time it takes to deliver the baby, 2 prior cesareans 8.5 minutes, and 3 prior cesareans 18.1 minutes. This delay can compromise the health of the baby, researchers concluded.
Association of caesarean delivery for first birth with placenta praevia and placental abruption in second pregnancy. (Yang, et al., British Journal of Obstetrics and Gynecology: 2007 May;114(5):609-13.)
Study Design: Researchers examined the incidence of placenta previa (placenta blocking the cervical opening) and placental abruption (placenta separating from the wall of the uterus prematurely) in women who have had a prior cesarean vs. a prior vaginal delivery.
Bottom line: Compared to vaginal birth, cesarean increased the risk of placenta previa by 47 percent and placental abruption by 40 percent. Both complications carry the risk of death for both mother and baby. Researchers indicated that complications may be due to the cesarean scar on the uterus.
Risks of adverse outcomes in the next birth after a first cesarean delivery. (Kennare, et al. American Journal of Obstetrics and Gynecology. 2007 Feb; 109(2 Pt 1):270-6.)
Study Design: Researchers examined the complication rate of women who delivered their first baby by cesarean vs. vaginally.
Bottom line: Women who had a prior cesarean delivery were more likely to have complications than women who had a prior vaginal delivery. Women with a prior cesarean were more likely to have a placenta previa (odds ratio [OR] = 1.66), placenta acreta (OR = 18.79), and bleeding during pregnancy (OR = 1.23). During delivery, women with a prior cesarean were also more likely to have a prolonged labor (OR = 5.89), uterine rupture (OR = 84.42), and need an emergency cesarean (OR = 9.37). Babies born to women with a prior cesarean were more likely to be small for their gestational age (OR = 1.12), have a low birth weight (OR = 1.30), and to be still born (OR = 1.56).
Safety and efficacy of vaginal birth after cesarean attempts at or beyond 40 weeks of gestation. (Coassolo, et al., Obstet Gynecol. 2006 Jan;107(1):205)
Study Design: Women who attempted VBAC before the estimated due date (EDD) were compared with those at or beyond 40 weeks of gestation.Researchers assessed the relationship between delivery after the EDD and VBAC failure or complication rate.
Bottom Line: The risk of uterine rupture (1.1 percent compared with 1.0 percent) or overall morbidity (2.7 percent compared with 2.1 percent) was not significantly increased in the women attempting VBAC beyond the EDD. Women beyond 40 weeks of gestation can safely attempt VBAC, although the risk of VBAC failure is increased. ( **Note from me…this is because of pressure from the OBs/Midwives…NOT because of the VBAC itself!** )
Incisional endometriomas after Cesarean section: a case series. (Minaglia, et al., J Reprod Med. 2007 Jul;52(7):630-4.)
Study Design: Patients were identified who were diagnosed with incisional endometriomas (functional endometrial tissue outside the uterine cavity, within the incision) after undergoing cesarean section.
Bottom Line: The overall incidence of incisional endometriomas following cesarean section was 0.08 percent. Optimal treatment is by surgical excision.
Predicting Failure of a Vaginal Birth Attempt After Cesarean Delivery. (Srinivas, et al., Journal of Obstetrics and Gynecology. 2007 Apr;109(4):800-5)
Study Design: Researchers analyzed the records of women offered VBAC in 17 community and university hospitals, to identify any factors that could be used to predict failure in attempting VBAC.
Bottom Line: Prelabor and labor factors cannot reliably predict VBAC failure.
Caesarean delivery and risk of stillbirth in subsequent pregnancy: a retrospective cohort study in an English population. (Gray, et al., BJOG:2007 March 114(3) 264-270)
Study Design: Researchers compared the incidence of stillbirth following a previous cesarean section with stillbirths following no previous cesarean section.
Bottom Line: Pregnancies in women following a pregnancy delivered by cesarean section are at an increased risk of stillbirth.
Predicting placental abruption and previa in women with a previous cesarean delivery. (Odibo, et al., Am J Perinatol. 2007 May;24(5):299-305.)
Study Design: In women with a previous cesarean section, researchers compared those who had a placental abruption and/or previa with those who did not.
Bottom Line: Three or more previous cesarean sections was a significant risk factor for placental abruption and previa.







