X-posted from my
NoNonsenseParenting Blog:
Sadly, many new parents do not even research circumcision. This is just as disappointing to me as when they choose to keep their sons intact, but do no research and therefore don't care properly for them. When we just blindly make decisions, especially those about our children's health (Vaccinations, elective surgeries, feeding, etc) we aren't just hurting ourselves, or our kids...but the population as a whole.
If you circumcise your son because it's "Just what everyone does" what other things are you going to alter in the name of popularity? Will you get your daughter a boob job in high school if "everyone else is doing it" according to rumor? Because that's all that myth is, a rumor. Roughly, only half of US boys are being circumcised today. In some areas, like the West Coast, that number is as low as 30%. But, I won't make an argument for something as important as circumcision based off of location. After all, perhaps you're on the East coast which boasts a disgustingly high circ rate of 90% in some areas. And after all, you may move someday.
I'd much rather convince you of the ill effects of infant circumcision with FACTS. To do so, I'm going to list common pros that are given in favor of circumcising young infant boys. Then, I'm going to explain why they're bull shit.
"My husband is circumcised, I don't want him to wonder why he doesn't look like daddy"-This is a very common reason for wanting to circumcise an infant. But, let's just think about this for a second. What other body parts of your husband's need to match? If your son's ears are different, are you going to alter them? No. And hey, your son won't have the same genitalia as you, but you'll explain that to him, that boys and girls look different. So why not explain to him that his daddy had a surgery as a baby to remove his skin, but you didn't do that to him because *insert whatever reason here, like "You were born perfect".* I can tell you that your son, if he has any questions at all about dad's privates, will probably be more interested in why he has pubic hair and why daddy's penis is bigger than his. You don't go around performing elective surgeries on people so they match. We're all different and unique...this should involve a life lesson, not scalpels.
"All his peers will be circumcised and I don't want him teased in the locker room."-If a child is going to be teased about something, there's little you can do to prevent it. He could be teased for having a small penis...you're not going to get it enlarged. Plus, this excuse works on the assumption that guys are going to be checking each other out in the locker room. In the rare event that someone were to poke fun at your kid for having a foreskin, there are many retorts your son could shoot back, like "Why are you checking out my junk, jealous?" or "At least I'm not lacking in that department and have my whole penis." There's no reason to alter your perfect infant because someday, someone in some random situation may tease him. Plus, I remind you that the circ rates are dropping, drastically. The boys of today are being left intact, much like the rest of the world (85% of the men in our world have their foreskins).
"Well, those two reasons aside, it's better for his health. It's cleaner, it's easier to clean and he won't spread STDs as easily."-No, no, and, no. To understand this you have to first understand how the
foreskin functions. In infant boys, the foreskin is fused to the glans (head of the penis) much like your finger nail is attached to your finger. When your baby pees, it flushes out the inner part of the foreskin (and remember that urine is sterile) so this works to keep your son clean. Also, by keeping his foreskin, you prevent feces from his diaper from touching his urethra or getting under his foreskin, and therefore, prevent the chance of him getting foreign bacteria in his urinary tract. Older studies suggested that circumcised boys were less likely to get UTIs. There are more studies that show no difference and others that show that intact boys get them less often. Regardless of what the truth is, girls are more prone to UTIs than either circumcised OR intact boys, and we treat them with proper hygiene and antibiotics, no surgery.
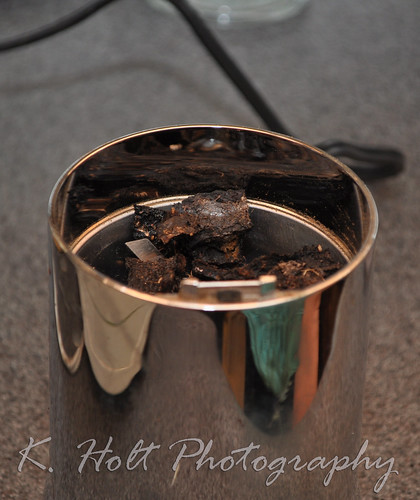
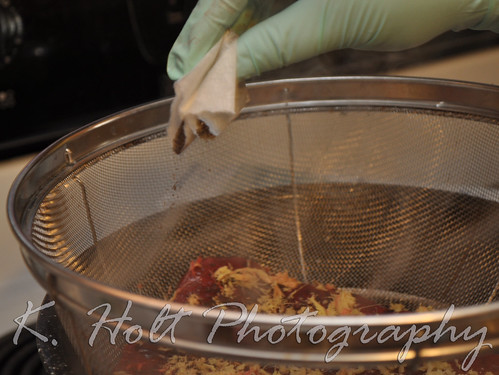
Now to clean, let's imagine this: An intact boy requires NO special care. Because the foreskin is fused to the glans, you do
NOT retract it, ever. This could cause pain, tears, and adhesions. Instead, you wipe only what you see, like you wash your finger. If you circumcise your infant, you'll have much more to do. During the healing process, you'll be taking care of a wound, in a diaper. Afterward, you'll have to clean any skin that was still left very thoroughly so that he doesn't get an infection. You may also have to worry about the freshly cut skin trying to heal back to the glans, usually resulting in
adhesions. Advice on this varies from "do not retract" (like in intact boys) to "you must retract to prevent the adhesions or break them" so there's really no TRUE information on what to do. When the intact boy retracts naturally (sometime between infancy and puberty, but most commonly toddlerhood) he can retract, rinse and replace at bathtime. No soaps, just water. No harder than if he lacked foreskin.
As far as STDs are concerned, no study really has the truth established. Those that say intact men are at greater risk, or rather carriers, of more infections (like HPV) are grossly incorrect and make little sense. The most commonly quoted study is about a group in Africa, where they taught the freshly circumcised men safe sex practices and provided them with condoms, but not the group they left intact. They also didn't factor that the freshly circumcised men weren't having sex while their penises healed. They found that the intact men contracted HIV more often than their cut counterparts, based on their poor approach of collecting this data. This study was, on top of it all, cut short (no pun intended). We can also look at the population of America and conclude this study makes no sense. Our own HIV/AIDS rate is quite high to that of other industrialized counter parts, yet, we have an astoundingly high circumcision rate (about 90% of grown men in the US are circumcised, as this was the rate about 20-some years ago). So, how is it that we have such a high rate of HIV/AIDS when we also have such a high rate of circumcision? That makes no sense...
On top of that, to argue in favor of surgery on infants, to possibly reduce the risk of STD transfer in adults is irresponsible. Instead, we need to teach our children how their bodies function, how STDs are transferred and contracted, and push safe sex. THIS is what will protect your son or daughter, not a false sense of protection because they were circumcised (or their partner is).
"But uncircumcised penises are soooo gross!"-Really? How attractive is
YOUR genitalia? If a man you were really in to took you home, and you started to fool around, and he caught a glimpse of your goods and never called you again because it was "so gross" he'd be labeled an asshole. Most genitals are not very attractive, female or male; circumcised or not. We are all made differently and none of us "match". To discount a person because they have foreskin is incredibly shallow. Just like a man discounting a woman for having an extended clitoris, longer labia, or not having her clitoral hood removed is shallow.
There is nothing gross about the state of a man's (or infant's) natural penis. This is how they are
SUPPOSE to look; without tight skin or dark circle scars. We tend to be afraid of what we don't know, but that doesn't make it's ok. It's just ignorance to how a penis is suppose to look. If your son's toes were oddly shaped and ugly, you wouldn't remove them. They are part of him, and you love every bit.
"Well, I've never actually seen one. I didn't mean it was gross looking because of the skin, I meant because of all that nasty stuff that builds up in there!"-If you've never seen one, how do you know it's nasty? Oh, because of rumors and stigmas surrounding intact men in America. Well, we're talking about infants, for one. Remember how I said the glans and foreskin were fused? Yea, there's nothing "building up". And, the "stuff" is called smegma. This is a natural lubricant produced by the body, you have it too. It's your discharge. It keeps your pH balance normal, it keeps you lubricated for sex, it keeps your skin there soft. Everyone needs to practice proper hygiene, circumcised men included. In the end, a dirty penis is a dirty penis. Most intact men take extra care to keep themselves clean, partly because there is such a stigma about having a foreskin. In order for smegma to build up, the man needs to really lack in caring for his man bits, and this would probably be no different if her were circumcised, and I doubt you'd put EITHER penises in your mouth. But again, we're talking about infants, and whether you need to worry about his for YOUR son...so again, the answer is no. For the first portion of his life, his foreskin is self cleaning, after that, you teach him how. After that, it's up to him whether he'll be a slob or a Mr. Clean kinda guy. Regardless, it's nothing to remove body parts over.
"If it was unnecessary, they wouldn't do it."-Many insurance companies, and state medicaid, are no longer covering circumcisions. Certain hospitals have banned the procedure as well. I've heard, first hand from friends/aquaintances, quotes in the range of $350-$1500 to have the surgery performed on their newborn. The reasons given "It is not medically necessary, it is a preference." My co-worker and I were discussing this issue one day. She was telling me that she had taken him (her son) to the pediatrician to get it done, because the hospital didn't perform the. The pediatrician told her the procedure was not covered by her insurance because it was considered a cosmetic surgery, and it would cost them $400. She debated it, but he told her that there was absolutely no reason to do it, that many boys today aren't getting circumcised, and told her proper care (not to retract). He's 5 and while her intentions walking in to the pediatricians office that day were to circumcise him without a thought or any research, she told me how happy she is that it wasn't covered and that he remained intact. I'm pretty sure he'll be happy about that, too!
If there are any other reasons you've heard for someone wanting to circumcise, I'd love to hear them. If you've been considering it and are still confused, have more questions, etc I would love to address that.
There are so many decisions for new parents to make, and it's important that you're informed. What I found when researching
circumcision was that
EVERY pro-circ benefit could be debunked with medical facts. That was enough for me. Why expose my perfect newborn boy to the risks of bleeding, pain, MRSA staph infection, decreased sensitivity and genital integrity if there were no benefits to it?
For a great first time parent article, check this out:
http://www.circumstitions.com/Itsaboy.htmlHere's a group of doctors opposing circumcision:
http://www.doctorsopposingcircumcision.org/For a quick, easy fact-checking decision maker, look at this:
http://circumcisiondecisionmaker.com/To find out why this group is fighting for baby boy's rights, go here:
http://www.intactamerica.org/Already raising an intact son (or pregnant with one who'll stay that way) join us here:
*Raising Intact Boys* on cafemom.